RESEARCH IMPACT
Celebrating a $108 Million Milestone in Hydrocephalus Research Funding
The Hydrocephalus Association (HA) is proud to celebrate a major milestone: more than $108 million has been invested into hydrocephalus research since our program began in 2009.
HA’s direct investment of $16 million has served as a critical catalyst, enabling our funded researchers and clinical networks to secure an additional $92 million in competitive grants from the National Institutes of Health (NIH), the Department of Defense (DOD), and other foundations. This incredible return on investment has fueled impactful research, including clinical trials and the development of potential drug therapies, offering hope to individuals living with hydrocephalus.
We are especially excited to recognize the continued success of our Innovator Award recipients, many of whom have recently secured substantial multi-million-dollar grants from the NIH and DOD. These awards validate the innovative and transformative ideas launched through our program and pave the way for deeper insights into the causes, treatment, and long-term management of hydrocephalus.
Thanks to the generosity of our donors and the dedication of our researchers, HA has become a driving force in advancing hydrocephalus research.
Successive Grant Support: National Institutes of Health

June Goto, PhD
Assistant Professor of Neurosurgery
Cincinnati Children’s Hospital Medical Center

Sheng Chih (Peter) Jin, PhD
Assistant Professor of Genetics and Pediatrics
Washington University in St. Louis

Maria Lehtinen, PhD
Professor, Hannah C Kinney
Chair in Pediatric Pathology Research
Boston Children’s Hospital, Harvard Medical School

Brandon Miller, MD, PhD
Associate Professor of Pediatric Neurosurgery
Medical University of South Carolina
Successive Grant Support: Department of Defense

Maria Bonilla Garcia, PhD
Assistant Professor of Neurosurgery
Virginia Commonwealth University

Carolyn Harris, PhD
Professor of Chemical
Engineering and Materials Science
Wayne State University
A Landmark Year in Award Expansion
The Hydrocephalus Association is proud to announce an unprecedented number of research funding awards in 2024, reflecting our commitment to advancing hydrocephalus research, fostering innovation, and expanding the research ecosystem.
In 2024, we were able to offer seven different types of prestigious awards. This is a testament to our mission of improving the lives of individuals affected by hydrocephalus by supporting researchers at various stages of their careers and across multiple disciplines.
2024 Funding Opportunities
Innovator Award
Accelerator Award
Next Generation Travel Award
Epidemiology Challenge Award
Neuropsychology & Cognition Award
Engineering in Hydrocephalus Prize
Cynthia Solomon Resident's Prize in Hydrocephalus

Innovator Awards: Catalyzing Bold Ideas
The Innovator Awards exemplify the power of creativity and early-stage innovation in hydrocephalus research. Designed to provide essential seed funding, these awards support visionary researchers in translating bold concepts into actionable projects. We are grateful for our continued partnerships with Team Hydro and the Rudi Schulte Research Institute (RSRI), whose collaboration makes these awards possible.
2024 Innovator Award Recipients
Mohammed Alshareef, BSE, MD
Assistant Professor in the School of Medicine at University of Colorado Denver
Complement Alternative Pathway Initiation Contributes to Post- Hemorrhagic Hydrocephalus in a Neonatal GMH Model

Peter Chiarelli, MD, PhD
Assistant Professor in the Department of Surgery, Division of Pediatrics at Children’s Hospital Los Angeles
Quantitative, Non-Invasive Shunt Flow Measurement for Improved Management of Shunted Hydrocephalus
Geoffrey Colby, MD, PhD
Professor in the Department of Neurosurgery at University of California, Los Angeles
Validation of a Novel Implantable Ventriculoperitoneal Shunt Flow Sensor
Cameron Sadegh, MD, PhD
Neurosurgeon and Assistant Professor in the Department of Neurological Surgery at UC Davis
Utilizing Neurosurgical Specimens to Study Intraventricular Hemorrhage and the Feasibility of Targeted Gene Therapy

Maria Garcia Bonilla, PhD
Assistant Professor of Pediatric Neurosurgery in the Department
Neurosurgery at Virginia Commonwealth University
Targeting Neuroinflammation in PHH: a Novel Immunomodulatory Approach

Mercedeh Javanbakht Movassagh, PhD
Associate Research Scientist (faculty role)
Department of Neurosurgery at Yale University
The Role of Pathogens and Non-Coding RNAs in Neonatal Hydrocephalus
Jennifer Kong, PhD
Assistant Professor of Biochemistry University of Washington
Leveraging a Cortical Spheroid System to Understand the Pathogenesis of Hydrocephalus
Accelerator Awards: Advancing Research in Treatments

In 2024, HA proudly launched the Accelerator Award, a new initiative aimed at helping established investigators advance promising work in hydrocephalus prevention or non-invasive treatment. Backed by the generous support of the Batterman Foundation and Team Hydro, this $85,000 award supports one-year projects that demonstrate clear potential to advance the current research to the next stage, such as transitioning from in vitro cell studies to animal models, from small to large animal models, or from animal studies to human clinical research. This award underscores HA’s strategic focus on moving treatment discoveries forward.
2024 Accelerator Award Recipients

Mark Johnson, MD, PhD
Professor and Chair, Neurological Surgery
University of Massachusetts Chan Medical School
Interplay Between Genetics and Alcohol Consumption in iNPH

Maria Lehtinen, PhD
Professor, Hannah C Kinney Chair in Pediatric Pathology Research, Boston Children’s Hospital
Harvard Medical School
A Large Animal Model of Germinal Matrix Hemorrhage for the Advancement of Choroid Plexus Therapies

Lauren Jantzie, PhD
Co-Principal Investigator
Associate Professor of Pediatrics, Neurology, and Neurosurgery, Johns Hopkins University Inflammatory Lipids as Targets & Biomarkers for Acquired Hydrocephalus
Shenandoah Robinson, MD
Co-Principal Investigator
Professor of Neurosurgery, Neurology and Pediatrics, Johns Hopkins University
Engineering in Hydrocephalus Prize: Inspiring the Next Generation of Innovators
Also new in 2024, the Engineering in Hydrocephalus Prize supports undergraduate and graduate research projects that explore engineering-based solutions to hydrocephalus. This initiative offers student engineers more than recognition, it connects them with expert mentors in bioengineering and hydrocephalus, and provides them with the opportunity to attend HA’s 2025 Engineering Research Workshop. This prize encourages diverse perspectives and creative problem-solving in hydrocephalus.

Haritosh Patel, BASc and Amy Huang, BASc
Test Bench Development for Enhancing Sensor and Catheter Design to Prevent Hydrocephalus Shunt Blockages

Yuli Wang, MS
Artificial Intelligence for Monitoring and Predicting Disease in Patients with Idiopathic Normal Pressure Hydrocephalus Using Imaging and Clinical Data

Bianka Valecruz
Test Bench Development for Enhancing Sensor and Catheter Design to Prevent Hydrocephalus Shunt Blockages
Next Generation Scientists Travel Award: Investing in Future Leaders
HA’s Next Generation Scientists Travel Award enabled 12 early-career researchers, including undergraduates, graduate students, postdoctoral fellows, and medical trainees, to participate in the 2024 National Conference on Hydrocephalus (HA CONNECT). This award supports the professional growth of emerging scientists by offering them a platform to present their research through oral and poster presentations, while fostering engagement with peers, mentors, and the hydrocephalus patient community. Through these interactions, participants gain perspective in hydrocephalus research and broaden their professional networks.
Timothy Heck, MD
Johns Hopkins University

Hawley Helmbrecht, PhD
Johns Hopkins University
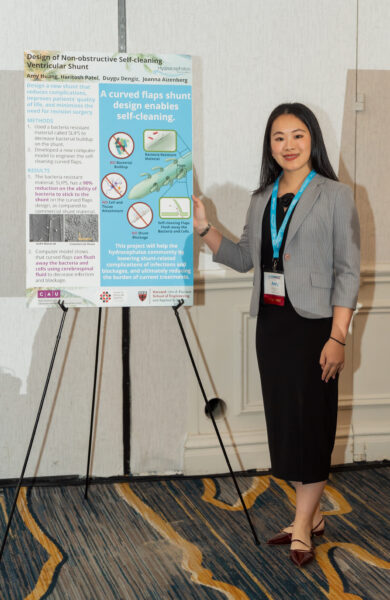
Amy Huang, BASc
University of Toronto
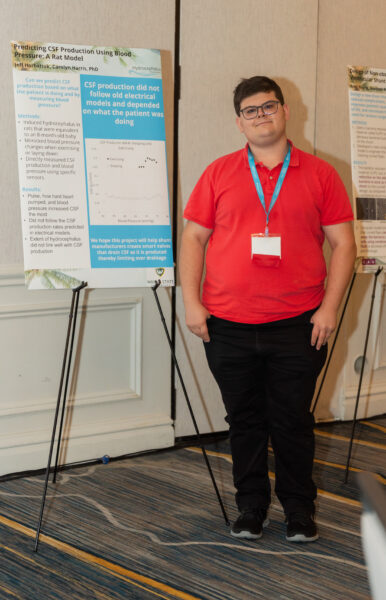
Jeffrey Horbatiuk, BS
Wayne State University

Verayna Newland, BS
Indiana University, Indianapolis
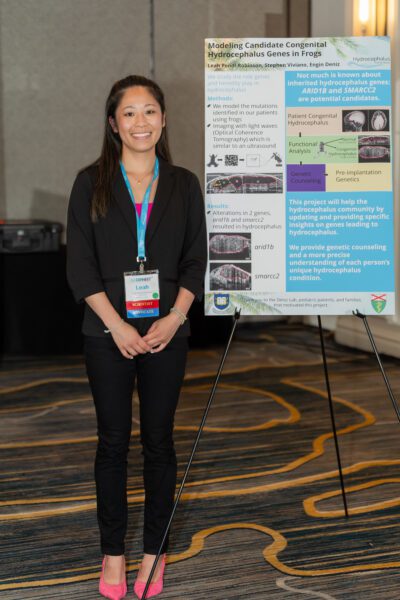
Leah Pendl-Robinson, BS
Yale University

Elizabeth Ricci, BS
Yale University

Christopher Roberts, MS
Wayne State University

Brady Rivkin
Carleton College

Riccardo Serra, MD
University of Maryland

Gwendolyn Sebring, BS
University of Cincinnati

Bianka Valecruz
University of North Dakota
Research Workshops: Shaping the Hydrocephalus Research Agenda
HA Hosts Two 2024 Research Workshops Focused on Advancing Hydrocephalus Treatments
 In 2024, the Hydrocephalus Association (HA), with support from the Rudi Schulte Research Institute and Cincinnati Children’s Hospital Medical Center, hosted two impactful research workshops aimed at accelerating progress in hydrocephalus treatment. The first focused on non-invasive therapies, such as drug-based approaches, and the second addressed idiopathic Normal Pressure Hydrocephalus (iNPH).
In 2024, the Hydrocephalus Association (HA), with support from the Rudi Schulte Research Institute and Cincinnati Children’s Hospital Medical Center, hosted two impactful research workshops aimed at accelerating progress in hydrocephalus treatment. The first focused on non-invasive therapies, such as drug-based approaches, and the second addressed idiopathic Normal Pressure Hydrocephalus (iNPH).
The non-invasive therapies workshop, held in Cincinnati, OH, brought together more than 75 scientists, clinicians, patients, and industry representatives. Building on the momentum from the 2023 workshop, this event focused on identifying research priorities that could move the field closer to clinical trials. Key sessions addressed the use of animal models, techniques for measuring outcomes, lessons learned from clinical trials, and the importance of cross-field collaboration. A patient panel also added an important real-world perspective on living with hydrocephalus and participating in research.
A major outcome of this workshop was a white paper titled Research Priorities for Non-Invasive Therapies to Improve Hydrocephalus Outcomes, published in the scientific journal, Fluids and Barriers of the CNS. The paper outlines strategic steps to transition promising research into viable, non-surgical treatment options. This publication serves as a roadmap for research across academia and industry.
HA's second workshop of 2024 turned the spotlight on iNPH, gathering experts across many disciplines to chart a long-term research agenda for the next 10 years. With many living with iNPH, the timing is critical to improve early diagnosis, treatment options, and patient care. The workshop highlighted innovations in diagnostics, especially the use of artificial intelligence (AI) and explored cerebrospinal fluid (CSF) dynamics, glymphatics, and biomarkers in disease progression and treatment.
Participants also heard from a panel of patients and caregivers, who shared deeply personal stories about the challenges of delayed diagnosis and care. These perspectives emphasized the need for a more patient-centered research agenda and improved support systems. The workshop's findings will be compiled into a white paper to guide the iNPH research community toward impactful, patient-informed solutions.
Together, these two workshops reflect HA’s continued leadership in uniting researchers, clinicians, and patient advocates to address urgent gaps in hydrocephalus research. By creating collaborative spaces for forward-thinking dialogue, HA is helping to drive research that can improve quality of life for those affected.
Clinical Research Networks
What Are Clinical Research Networks? A Look at HCRN and AHCRN in Action
Clinical research networks are collaborative groups of hospitals, physicians, and researchers who work together to conduct multi-center studies aimed at improving patient care and understanding the clinical aspects of hydrocephalus. By pooling data, expertise, and resources, these networks are able to answer complex clinical questions more effectively and analyze evidence that can guide best practices in diagnosis, treatment, and outcomes.
The Hydrocephalus Association proudly supports two such networks: the Hydrocephalus Clinical Research Network (HCRN) for pediatric patients and the Adult Hydrocephalus Clinical Research Network (AHCRN). The HCRN focuses on improving care for children with hydrocephalus and is currently conducting the ESTHI clinical trial (see below), while the AHCRN is dedicated to improving treatment for individuals living with iNPH through the PENS clinical trial (see below). These networks are both vital to understanding hydrocephalus across the lifespan.
Leadership Transition at HCRN: Dr. William Whitehead Named New Chair
 In 2024, the Hydrocephalus Clinical Research Network (HCRN) underwent a leadership transition as Dr. William (Bill) Whitehead, assumed the role of Chair. Dr. Whitehead brings deep clinical expertise and a strong commitment to advancing outcomes for children with hydrocephalus as a pediatric neurosurgeon at Texas Children’s Hospital and Professor of Neurosurgery at Baylor College of Medicine. His work focuses on improving surgical treatments and developing innovative approaches to care. With extensive experience in both clinical practice and research, Dr. Whitehead is well-positioned to guide the HCRN into its next chapter of growth and discovery.
In 2024, the Hydrocephalus Clinical Research Network (HCRN) underwent a leadership transition as Dr. William (Bill) Whitehead, assumed the role of Chair. Dr. Whitehead brings deep clinical expertise and a strong commitment to advancing outcomes for children with hydrocephalus as a pediatric neurosurgeon at Texas Children’s Hospital and Professor of Neurosurgery at Baylor College of Medicine. His work focuses on improving surgical treatments and developing innovative approaches to care. With extensive experience in both clinical practice and research, Dr. Whitehead is well-positioned to guide the HCRN into its next chapter of growth and discovery.
Dr. Whitehead succeeds Dr. John Kestle, the founding Chair of the HCRN, who stepped down after more than a decade and a half of groundbreaking leadership. Under Dr. Kestle’s direction, the HCRN became a leading collaborative network that has transformed hydrocephalus research producing some of the most impactful studies in the field. The Hydrocephalus Association is deeply grateful to Dr. Kestle for his leadership and looks forward to continued collaboration under Dr. Whitehead’s direction.
"The HCRN and AHCRN are comprised of impressive clinician scientists who genuinely care about improving patient outcomes. While meeting in Seattle, I was deeply moved when our AHCRN investigators suggested we stop by Locust Cider to show their gratitude for the more than $130,000 Locust Cider has contributed to HA’s mission.” — Diana Gray, President and CEO
Clinical Trial Updates
PENS: Landmark Trial Nears Completion in Study of Shunting for iNPH
The Placebo-Controlled Efficacy in idiopathic Normal Pressure Hydrocephalus Shunting (PENS) clinical trial, a multi-center trial led by Dr. Mark Luciano at Johns Hopkins, is concluding, and investigators expect to publish results within the next year.
The PENS trial is significant for individuals with idiopathic Normal Pressure Hydrocephalus (iNPH) because it is the first to rigorously evaluate the efficacy of shunting using a blinded, randomized design. Despite shunting being a common treatment, the PENS trial has the potential to greatly improve decision-making, reduce unnecessary procedures, and ensure that patients most likely to benefit from shunting receive the right care.
Backed by a record-breaking $14 million grant from the NIH’s National Institute of Neurological Disorders and Stroke (NINDS), PENS is the first large-scale, multi-center, blinded, randomized controlled trial evaluating the effectiveness of shunting for iNPH. Conducted at 21 sites across the U.S., Canada, and Sweden including eight within the Adult Hydrocephalus Clinical Research Network (AHCRN), PENS represents a major milestone in iNPH research.
Comparing Hydrocephalus Treatments in Infants: ESTHI Trial Reaches 130 Participants
The Hydrocephalus Clinical Research Network (HCRN) is currently conducting a large randomized controlled clinical trial to compare two common treatments for hydrocephalus in infants. The study, Endoscopic versus Shunt Treatment of Hydrocephalus in Infants (ESTHI), has now enrolled 130 participants across participating centers.
The National Institute of Neurological Disorders and Stroke (NINDS) at the National Institutes of Health (NIH) awarded support for the ESTHI in September 2019. The primary goal of the trial is to evaluate if traditional shunt placement or endoscopic third ventriculostomy with choroid plexus cauterization (ETV+CPC) results in better cognitive outcomes for infants diagnosed with hydrocephalus.
Shunt placement has long been the mainstay treatment for hydrocephalus. ETV+CPC is an alternative technique that reroutes fluid internally without the use of a shunt device and it also reduces CSF production. Even though both procedures are widely used, there is no evidence indicating which offers better long-term cognitive outcomes.
By comparing these two approaches, the ESTHI trial aims to provide clarity to guide pediatric neurosurgeons and improve decision-making for families facing a hydrocephalus diagnosis. This trial reflects a dedication to improve long-term outcomes for infants affected by this condition.
SCEMPI Clinical Trial Recruiting Preterm Infants with Severe IVH
Drs. Shenandoah Robinson and Lauren Jantzie at Johns Hopkins are leading the first clinical trial to test a drug combination treatment in preterm infants. The Safety of Combined Therapy with Erythropoietin & Melatonin for Preterm Infants with Intraventricular Hemorrhage (SCEMPI) is a blinded, randomized controlled clinical trial designed to evaluate the safety of combining high-dose melatonin and erythropoietin (EPO) in very preterm infants diagnosed with severe intraventricular hemorrhage (IVH). The primary objective is to assess safety along with tracking the incidence of other comorbidities associated with severe IVH in this vulnerable population.
The SCEMPI clinical trial has started and is now enrolling participants. Recruitment has successfully started with five preterm infants enrolled.
Eligible participants are preterm infants born between 23-0/7 and 31-6/7 weeks of gestation, less than 21 days old, and diagnosed with at least unilateral grade III IVH on a head ultrasound performed within the first 5 days of life.
The drug treatment is a high-dose melatonin and EPO, both administered until 34 weeks of age. Safety is closely monitored throughout the treatment period and beyond. All clinical personnel and families are blinded to treatment assignment, except for the research pharmacy.
SCEMPI is supported by funding from the NIH NICHD and the Johns Hopkins Children’s Center.
HA Publishes Key Research Priorities to Improve Cognitive and Neuropsychological Outcomes
 The HA has published a landmark paper outlining important research priorities aimed at improving cognitive and psychological outcomes for individuals living with hydrocephalus. The paper, titled Research Priorities for Improving Cognitive and Neuropsychological Outcomes in Hydrocephalus, was published in Fluids and Barriers of the CNS in 2024 and represents the outcome of a dedicated research workshop held in Houston, TX in collaboration with the Rudi Schulte Research Institute.
The HA has published a landmark paper outlining important research priorities aimed at improving cognitive and psychological outcomes for individuals living with hydrocephalus. The paper, titled Research Priorities for Improving Cognitive and Neuropsychological Outcomes in Hydrocephalus, was published in Fluids and Barriers of the CNS in 2024 and represents the outcome of a dedicated research workshop held in Houston, TX in collaboration with the Rudi Schulte Research Institute.
This workshop brought together a multidisciplinary group of experts including neurosurgeons, neuropsychologists, neurologists, scientists, and individuals with lived experiences, to tackle one of the most persistent challenges in hydrocephalus care: the cognitive and neuropsychological impacts of the condition across the lifespan. Guided by results from a community-driven research prioritization effort and developed through months of collaborative planning, the workshop focused on identifying research gaps and establishing a shared agenda to guide future inquiry.
The resulting paper outlines four central areas where focused research is needed: (1) understanding neuropsychological phenotypes, (2) developing treatment-focused research strategies, (3) improving preclinical and translational tools, and (4) building systems for longitudinal cognitive care. These priorities aim to bridge scientific gaps and ultimately enhance the daily lives and functional independence of people living with hydrocephalus.
As cognitive and quality-of-life outcomes remain under-addressed in hydrocephalus care, HA is proud to help shape a national research agenda focused on this critical aspect of patient well-being and quality of life.
Growing the Ecosystem
Engineering Outreach for Better Hydrocephalus Treatments
As part of its strategic plan, the Hydrocephalus Association (HA) is expanding its research network by actively engaging bioengineers in hydrocephalus research. While doctors and scientists have long led the charge, HA is now reaching out to engineering students and faculty to inspire fresh thinking and innovative device development. Shunt failure remains a persistent issue in hydrocephalus treatment and the HA is reaching out to engineers to reimagine solutions that could improve outcomes for patients.
In the outreach in 2024, Dr. Carolyn Harris of Wayne State University joined HA’s Jennifer Bechard, HA’s Jason Preston, Dr. Michael Siegel, Dr. Michael Williams, and Dr. Monica Chau to present pressing research challenges to bioengineering students and faculty at the University of Michigan and the University of Washington. Their presentations spanned several bioengineering classes and a department-wide seminar, highlighting technical issues like fluid flow and shunt disconnection, while also centering the lived experiences of individuals with hydrocephalus.
To spark innovation, HA awarded three engineering student teams for hydrocephalus-focused projects and will continue this initiative in 2025. By investing in the next generation of engineers, HA hopes to accelerate the development of smarter, more reliable treatment solutions—and move closer to a world without the burden of repeated neurosurgeries.